Kariesscreentest
Kariesscreentest is carried out to detect the bacterial count of lactobacilli and streptococcus mutans. Low bacterial counts represent a low risk of caries, high bacterial counts represent a high risk of caries. Based on the result – and other, non-bacteriological risk parameters – the patient decides with the support of the doctor which of the following therapeutic measures should be taken.
The basic recommendation in the S2k-Leitlinie caries prophylaxis for permanent teeth is that patients with an increased risk of caries are recommended to participate in structured prophylaxis programs. The investigation of subclinical risk parameters opens up this possibility of diagnosis-based individual prophylaxis (DIP), as also proposed by Prof. Dr. Zimmer.
If you are not sure, open the 4 risk options and determine the risk based on the microbiological findings and the further non-bacteriological saliva parameters.
LOW RISK
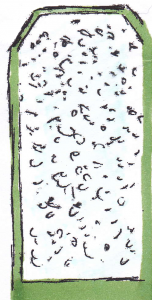
Lactobacilli*

Streptococcus mutans*
*Graphical representation of the results
Microbiological findings Low level of infection with streptococcus mutans in connection with low lactobacillus numbers.
Interpretation
Low risk of caries, further remedial measures possible.
Therapy
Professional measures:
- Regular check-ups in the dental practice
- Basic prophylaxis (1 – 2 times a year)
- Caries risk determination every 3 years
- Measures in the event of insufficient buffer capacity or secretion rate
- Regular x-ray check every 3 years
- Regular re-evaluation of the individual risk of caries, especially in the case of changing living conditions or changing conditions in the oral system (increased tooth eruption in adolescents)
- Prevention of root caries in exposed tooth necks
- Basic prevention
• Oral hygiene status
• Education and motivation
• Local fluoridation (e.g. Fluor Protector)
• Professional tooth cleaning (e.g. Proxyt)
Domestic measures:
- Adequate oral hygiene including proximal surfaces
- Use of fluoride-containing auxiliary products, e.g. use of table salt containing fluoride or fluoride gel
- Maintain eating habits
- Note exposed root surfaces
RISK
Lactobacilli*
Streptococcus mutans*
Lactobacilli*

Streptococcus mutans*
*Graphical representation of the results
Microbiological finding
Very high level of infection with mutans streptococci in combination with low lactobacillus numbers.
Low level of infection with streptococcus mutans,
high lactobacillus numbers.
Interpretation
High level of infection with streptococcus mutans, low lactobacillus numbers.
High level of infection with mutans streptococci (may include hygiene deficits, retention niches such as poor restoration design, deep fissures and dimples, morphological weak points) with presumably low sugar consumption.
Insufficient buffer capacity and / or an insufficient secretion rate have a strong risk-increasing effect. Further remedial measures are only possible to a limited extent and should only be carried out when the reasons of the increased streptococcus mutans content of the saliva have been found and treated.
Therapy
- Regular check-ups in the dental practice
- Basic prophylaxis (2 – 4 times a year), more often if lactobacillus numbers are high
- Measures in case of insufficient buffer capacity or secretion rate
- Check for root caries
- Control of sugar impulses and recommendation of sugar substitutes
- Examination of plaque predilection sites for their proportion of mutans streptococci with proven caries activity (circumscribed demineralized area)
- Application of chlorhexidine-containing varnishes necessary, every 8 weeks to 3 months (40% CHX varnish) once a month
- Regular X-ray checks (especially in adolescents bitewing images)
- Prevention of fissure caries
- Follow-up examination of microbiological saliva parameters after 1/2 to 1 year
- Optimal oral hygiene and approximate hygiene
- Control of exposed root surfaces
- Prevention of root caries
- Checking for gingivitis
- Application of chlorhexidine-containing varnishes in approximate spaces, on risk areas and plaque predilection sites (edge design of restorations, morphological weak spots, misaligned teeth, deficient oral hygiene areas [influencing the speed of recolonization])
- Application of varnishes / gels containing chlorhexidine
- Carrying out an intensive therapy to reduce the amount of caries-relevant germs using an application aid
- Use of a tin fluoride preparation
- Prevention of fissure caries (children and adolescents, also in deciduous dentition)
- Fissure sealing of all discolored or intact fissure systems (removal of all discoloration (minimally invasive procedure)
- Regular X-ray check (especially in adolescents bitewing)
- Follow-up examination of microbiological saliva parameters six months after completion of intensive therapy
- Information (pregnant women / young mother) about transmission routes and transmission prevention
- Measures of primary-primary prophylaxis
- Optimal smooth surfaces and approximal space hygiene
- Use of fluoride-containing auxiliary products
- Use of table salt or fluoride gel containing fluoride (in particular compounds containing tin fluoride and / or amine fluoride)
- Strong restriction of the number of sugar impulses (not more than 3 per day) using sugar substitutes, especially after domestic or professional chorhexidine applications
- Prevention of root caries
- Domestic measures with insufficient buffer capacity or secretion rate
HIGH
RISK
Lactobacillus*
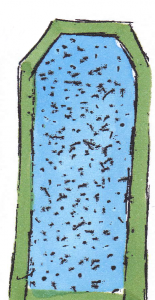
Streptococcus mutans*
*Graphical representation of the results
Microbiological finding Very high level of infection with mutans streptococci in combination with very high lactobacillus numbers.
Interpretation
High risk of caries on all tooth surfaces including the smooth surfaces also on the gumline area and the approximal spaces.
Therapy
- Regular check-ups in the dental office
- Basic prophylaxis (every 2 month)
- Professional tooth cleaning (with CHX-gel)
- Measures in case of insufficient buffer capacity or secretion rate
- Check for root caries
- Optimal oral hygiene and approximal hygiene
- Intensified nutritional counseling
- Control of sugar impulses and recommendation of sugar substitutes
- Control of exposed root surfaces
- Application of chlorhexidine-containing varnishes in approximal spaces and on risk areas and plaque predilection sites (edge design of restorations, morphological weak spots, misaligned teeth, deficient oral hygiene areas [speed of recolonization])
- Application of varnishes / gels containing chlorhexidine
- Carrying out an intensive therapy to reduce the amount of caries-relevant germs using an application aid
- Use of a tin fluoride preparation
- Regular X-ray check (especially in adolescents bitewing images)
- Prevention of fissure caries (children and adolescents, also in deciduous dentition)
- Fissure sealing of all discolored or intact fissure systems (removal of all discoloration (minimally invasive procedure)
- Prevention of root caries
- Checking for gingivitis
- Follow-up examination of microbiological saliva parameters six months after completion of intensive therapy
- Intensified controls of caries activity and success control
- Information (pregnant women/young mother) about the transmission routes and transmission prevention
- Measures of primary-primary prophylaxis
- Intensification of oral hygiene measures including approximal hygiene by floss
- Use of oral hygiene aids containing fluoride or tin fluoride
- Regular use of gels containing amine and / or tin fluoride
- Use of table salt or fluoride gel containing fluoride (in particular compounds containing tin fluoride and / or amine fluoride)
- Strong limitation of the number of sugar impulses (not more than 3 per day) using sugar substitutes (including chewing gum containing xylitol), especially following domestic or professional chlorhexidine applications (influencing the rate of recolonization)
- Domestic measures with insufficient buffer capacity
- Prevention of root caries
- Domestic measures with insufficient buffer capacity or secretion rate
- Measures of primary-primary prophylaxis
Buffer capacity
Findings
Interpretation
Therapy
pH › 5. A very good or good buffer capacity is an expression of a good defense situation in the oral cavity. This means that, especially when the saliva flow rate is extremely good, the oral biotope can build a good line of defense against food and plaque acids up to certain limits.
No therapy necessary
- Application of fluoride-containing varnishes to protect against enamel caries and root caries
- Additional application of varnishes containing chlorhexidine to protect against enamel caries and root caries
- Use of toothpastes containing bicarbonate
- Use of application aids
- Intensification of dental care measures, in particular professional tooth cleaning measures and recall intervals
- Check for halitosis
- Further measures for the therapy of hypo salivation / xerostomia with an extremely low memory flow rate (below 0,5ml/min)
- Checking for side effects of extensive medication (consequences of systemic medication)
- Secretion-promoting measures: use of chewing gum containing xylitol 3 times a day, 2 pieces for 5 min
- Gustatory stimulation by sugar-free lozenges
- Increasing saliva flow rate by adequate chewing behavior
- Reduction of acidic food and drinks
- Fundamental reduction of cariogenic snacks
- Chewable nutrition
- Toothpastes with sodium bicarbonate
- Regular application of fluoride rinses or fluoride gels in application aids (drug carriers) 2 times a week 5 min. If saliva flow is strongly reduced (‹0,5ml/min) once or twice a day
- Application of saliva substitutes
- Adequate hydration
- Measures for therapy of any existing halitosis
Secretion rate

Findings
›1ml/min
= 1ml/min
‹0,5 ml/min
Interpretation
Very good secretion rate
Good secretion rate
Poor secretion rate. No sufficient clearance rate, increased plaque formation, periodontal problems, foetor ex ore, high risk of caries, general medical anamnesis (medication)
Therapy
No therapy necessary
No therapy necessary
CHX varnishes / gels, application aids for fluoride varnishes, chewing activity (nutrition, chewing gum),
saliva substitution products (Saliva Natura, Aldiamed e.g.)
preventional appointments more often (considering all findings up to 4 times / annually
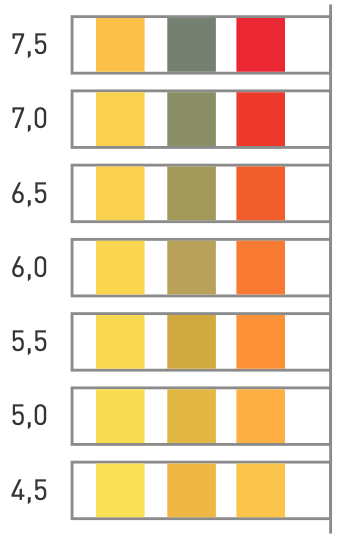
Saliva pH
Findings
Interpretation
Therapy
› pH7
‹ pH7
Good saliva pH
Unfavorable saliva pH value, risk of exposed root surfaces, general risk of caries
No therapy necessary
Measures to protect tooth necks, CHX varnishes / gels, fluoridation concept (varnishes, gels, intensified preventive care)
